With the global pandemic occurring in the year 2020, it was quite tough for every industry to cope with it. But where a lot of the industry suffered, the medical industry took this opportunity to improve its services and earn more amount of revenue. Not only did the industry leaders understand this time to be the best time to improve upon their area of innovation but a lot of automation and robotic processing automation (RPA), intelligent automation and artificial intelligence (AI) was used extensively during the revenue cycle management (RCM).
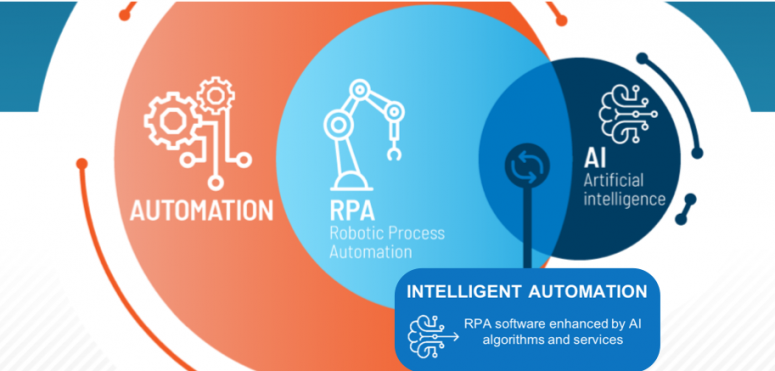
Intelligent Process Automation (IPA), Artificial Intelligence (AI) and Robotic Process Automation (RPA) have been engaging the interest of a lot of healthcare organizations and for good reason too. When it comes to revenue cycle management healthcare, intelligent automation helps in the streamlining of the entire process. They help medical organizations to improve upon their overall efficiency and also reduce the collection cost which ultimately results in the improvement of the cash flow for the organization. More cash flow equals a rise in the profit margins for the hospitals.
The revenue cycle management services approach tends to be compliant when it comes to the overall improvement process when using robotic process automation since it mostly emphasizes on statistics and workflow. For instance, let’s take an example, in regard to the accounts receivable, robotic process automation plays a key role since it helps in driving up the efficiency of the hospital and also levels up the effort that is required to accumulate the payment from patients and payers.
Upstream processes also get streamlined such as authorization and eligibility. When these are combined in a unified platform along with all the sophisticated analytics, then the result of the robotic process automation on the entire financial returns to the medical providers both small and large can be quite significant in nature.
As commercial and government payers lessen the reimbursement rates and the medical providers are obligated to maintain, in obedience, with a baffling arrangement of evolving and new regulations, the requirement for robotic process automation to preside over these challenges have been quite considerable. There have been only a few means when it comes to overcoming these challenges without the need for additional complexity or cost for that matter. One of the proven ways to fulfill this said goal with maximum benefits has been to leverage RPA in order to improve upon the revenue cycle management services.
BOTs form a digital layer on the already existing financial management and EHR (Electronic Health Record) to gain control of the often time-consuming and repetitive tasks that exist within the revenue cycle processes. These BOTs tend to function seamlessly across the entire organization in complete euphony with the staff. This results in achieving a higher amount of efficiency and productivity.

Insurance and eligibility discovery are crucial steps when it comes to creating clean claims that tend to have the top-most potential for insurance payments. These key elements are also significant when it comes to the management of the accounts receivable process. When you get to see the eligibility in real-time within the work system, it acts as an added advantage to speed up the revenue cycle management solutions.
While many clearinghouses and systems tend to offer this particular benefit when used together with the robotic process automation, the data and results tend to be very supportive and comprehensive of an efficient and robust claims management process.
The BOT driven process helps in providing precise and actual data with little to no manual intervention thereby reducing the time spent on handling incomplete claims or rejected claims. The robotic process automation (RPA) bots can quite quickly and easily search large volumes of insurance payer data for all the available benefits and coverages. This allows for the easier and better filing of claims when it’s being done for the first time thereby reducing the chances of claim denials due to misinformation. This becomes particularly crucial when it comes to the coverage of information since it might not always be readily accessible.
There are a lot of intricacies and complexities that are present within the revenue cycle management in medical billing, which needs to be dealt with in a proper manner if hospitals want an improvement in their profit margin. Some of these intricacies include incomplete or missing clinical documentation, financial clearance, patient collections, incomplete statements from patients, coding complications because of manual intervention and much more.
Incomplete or missing documentation can result in many problems regarding the claim denials or the reimbursement of claims. Mistakes that occur in these steps or anywhere during the medical billing procedure can mess up the entire revenue cycle thereby hurting the financial health of the medical providers. If healthcare organizations want to recover from the loos of their financial wealth, eliminating errors and taming the intricate yet complex elements present with the revenue cycle is of vital importance. Intelligent automation (IA) solutions can always act as an aid when it comes to this.
While robotic automation can transform the entirety of the revenue cycle, a complete evaluation of the already existing workflow and processes is crucial in order to start. This requires expertise in revenue cycle management in medical billing. Because even though the majority of the revenue cycle processes depend on the proper functioning of the revenue cycle. Also, for proper optimization, it still requires manual intervention even though it can be completely automated.
Therefore, understanding the things that do not require automation is therefore important. RCM IA ecosystem and R1 specialists tend to do all of the above. The end-to-end platform, therefore, helps in digitizing the revenue cycle, improving performance margin, freeing up staff and much more.
It is no surprise that information technology has therefore transformed healthcare in many of the areas thereby enhancing the overall experience of the patients. Companies like Synergy HCLS are doing a great job in providing top-notch medical billing services to the healthcare industry.
You cannot copy content of this page