Summary:
Master the medical billing cycle with our step-by-step guide covering key stages, expert tips, and various billing types. Learn how a well-managed revenue process boosts reimbursements, reduces denials, and strengthens healthcare finances.
We see the medical billing cycle as more than just paperwork. It’s a key driver of revenue in healthcare organizations. The process begins before the patient comes in and ends when all payments are made and recorded. When done right, it can make operations better, speed up reimbursements, and cut financial risks.
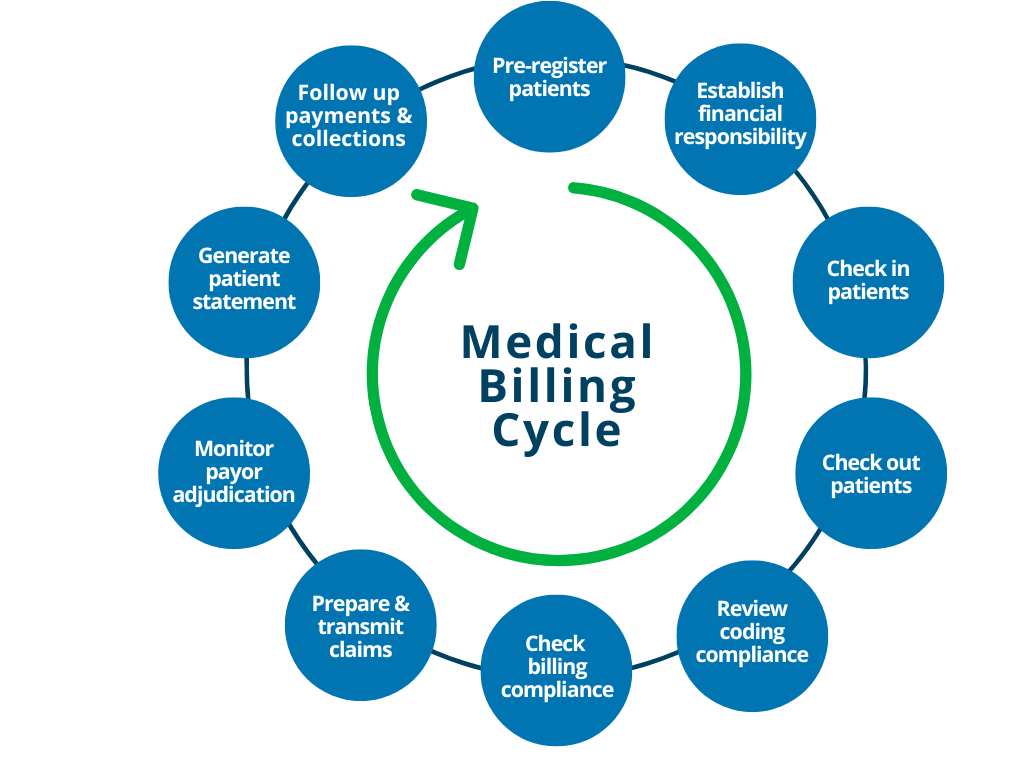
In this detailed guide, we present a comprehensive view of the 10 steps in the medical billing cycle. Each section gives useful tips for billing teams, revenue cycle managers, and healthcare admins. These insights help improve workflows and boost returns. We also cover medical billing types. This shows the main differences that change billing formats, coding systems, and payment routes.
10 Steps in the Medical Billing Cycle
Step 1: Patient Scheduling and Pre-Registration
We begin the medical billing cycle by gathering data. Before the patient shows up, we collect and validate key details:
- Patient demographics:
- Name
- Date of Birth (DOB)
- Address
- Phone
- Insurance policy details:
- Payer name
- Group number
- Policy number
- Plan type
- Identification documents: government ID, referral information
- Primary care provider and reason for visit
Completing this step early helps us avoid delays at the front desk. It also makes it easy to move on to the next steps. First, check if you qualify. Then, get approval.
This step sets the tone for the entire medical billing cycle. Errors can cause claims to be denied, lead to delays, and upset patients.
Step 2: Insurance Eligibility and Benefits Verification
Checking coverage early is key to smooth billing. We use EDI tools, payer portals, or clearinghouses to confirm:
- Active status of the policy
- Service-specific coverage, like:
- Physical therapy
- Imaging
- Lab work
- Copayments, coinsurance, and deductibles
- Referrals or pre-authorizations required
- Out-of-network implications
We automate this process when we can. This helps us be faster, more consistent, and scalable. Eligibility checks boost cash flow and help build trust with patients. It sets clear financial expectations.
Step 3: Pre-Authorization and Medical Necessity Confirmation
Many payers need approval for specific services. This covers surgeries, advanced diagnostics, and specialty consultations. We gather:
- Medical necessity documents include:
- Previous test results
- Progress notes
- ICD-10 codes matching payer policy guidelines
- Prior authorization numbers from payers
This step is administrative, but it is key to moving the medical billing cycle forward. Not getting the right authorization can mean unpaid claims. This condition applies even to services already provided.
Step 4: Patient Encounter and Service Documentation
Providers must document the clinical encounter thoroughly at the time of service. We train physicians and staff to include:
- Chief complaint and reason for the visit
- History of present illness
- Physical exam findings
- Procedures performed and time spent
- Discharge instructions and follow-up recommendations
This documentation helps with accurate billing. It also makes sure to follow payer rules and legal standards. Clear documentation is key for medical billing in healthcare settings.
Step 5: Medical Coding and Charge Capture
We turn provider documentation into billable code sets by using:
- ICD-10-CM: For diagnoses
- CPT/HCPCS: For procedures and services
- Modifiers help indicate special cases, such as:
- Bilateral procedures
- Repeat services
Coders look at charts or EHR exports. They then assign the right codes. Mistakes such as upcoding, undercoding, or omissions can lead to audits, fines, and lost income.
We also use charge capture software. It spots errors and ensures all services are included. Coders learn to handle two types of medical billing. Coding rules vary for outpatient and inpatient settings.
Step 6: Claim Generation and Scrubbing
Claims are generated in ANSI 837 format for electronic transmission. Before submission, we apply rigorous scrubbing protocols:
- Missing fields (e.g., NPI, place of service, referring provider)
- Invalid codes or non-covered services
- Incorrect patient information or payer details
- Bundling/unbundling errors
We use claim scrubbers and rule engines for each payer. We also conduct compliance audits. These tools help us find and fix issues before submission.
A clean claim speeds up the medical billing cycle. It cuts down rejections and raises first-pass acceptance rates.
Step 7: Claim Submission and Payer Transmission
We send claims electronically. You can do this through clearing houses or by paying the payers directly. We closely watch submission timelines. Such monitoring helps us meet payer deadlines. It also helps us avoid claim expiration.
Each claim includes:
- Provider credentials (NPI, TIN, taxonomy)
- Patient and policyholder info
- Date(s) of service
- Charges and codes
- Prior authorization numbers (if applicable)
We modify file formats and workflows for handling claims. The modification applies to both types of medical billing: institutional and professional. UB-04 for institutional claims, CMS-1500 for professionals.
Step 8: Payer Adjudication and Remittance
Payers process claims based on:
- Contracted fee schedules
- Medical necessity validation
- Network participation status
- Coverage limits and policy rules
They respond with:
- Remittance Advice (RA) or Electronic Remittance Advice (ERA)
- Explanation of Benefits (EOB)
We record payments in the practice management system. We also apply patient responsibilities and flag any underpayments or denials.
This step shows the financial result of the medical billing cycle. Every detail counts.
Step 9: Denial Management and Appeals
If claims are denied, we investigate, correct, and resubmit. Common denial reasons include:
- Missing modifiers or incorrect POS codes
- Invalid or expired authorizations
- Demographic mismatches
- Coverage exclusions
We sort denials by reason code. We also track trends and escalate when needed. Appeals consist of corrected claims, appeal letters, and extra documents.
A good denial management process cuts AR aging and speeds up cash flow in both kinds of medical billing.
Step 10: Patient Billing, Collections, and Financial Reporting
Once payments from payers are settled, we bill patients for any balances. This covers deductibles, copays, and any services that aren’t included. This includes:
- Printed or electronic statements
- Payment portals and automated reminders
- Financial hardship programs
- Third-party collection hand-offs (if necessary)
Finally, we generate reports on:
- Days in Accounts Receivable
- Net collection rate
- Denial rates and appeal success
- Patient payment ratios
These analytics help improve the medical billing cycle. They impact training, software updates, and compliance checks.
Is your billing team struggling with claim denials, slow payments, or compliance risks?
Let our experts improve each step of your medical billing cycle. We take care of coding, collections, and billing for both professionals and institutions.
Types of Medical Billing Cycle
Medical billing cycle can be categorized into various types based on the healthcare services provided and the payment structures involved. Here are the primary types of medical billing:
1. Professional Billing
- Used by: Physicians, therapists, individual providers
- Forms: CMS-1500
- Codes: CPT/HCPCS for procedures, ICD-10 for diagnosis
- Focus: Ambulatory/outpatient care
2. Institutional Billing
- Used by: Hospitals, SNFs, inpatient facilities
- Forms: UB-04
- Codes: Revenue codes, ICD-10-CM, and ICD-10-PCS
- Focus: Inpatient and facility-based services
3. Ambulatory Surgical Center (ASC) Billing:
- BILLING, Provider-based practitioners who perform surgical procedures in outpatient surgery facilities.
- Includes some professional and institutional billing components.
4. Durable Medical Equipment (DME) Billing:
- Focuses on billing for medical equipment and supplies, such as wheelchairs, crutches, and oxygen tanks.
- Requires adherence to specific regulations and documentation requirements.
5. Behavioral Health Billing:
- Related to therapists, such as psychiatrists, psychologists, and counselors.
- This includes unique coding and billing requirements for mental health services.
6. Dental Billing:
- Covers services provided by dentists and dental hygienists.
- Uses CDT (Current Dental Terminology) codes for billing dental procedures.
7. Radiology Billing:
- Involves billing for imaging services, such as X-rays, MRIs, and CT scans.
- Requires accurate coding for both technical and professional components of radiology services.
8. Pathology Billing:
- Concentrates on billing for lab tests and pathology services.
- Includes specific coding for those diagnostic tests and pathology readings.
Conclusion
We manage every part of the medical billing cycle with great care. Every step matters, from intake to getting payments from patients. Coding and compliance also play key roles. They work together to keep your revenue pipeline strong. Knowing the types of medical billing is important. This applies to both institutional and professional billing. Understanding how they apply within the cycle is essential.
Our process ensures reimbursement. It helps keep your healthcare organization financially strong over time.


